Why antibiotics can change digestion fast
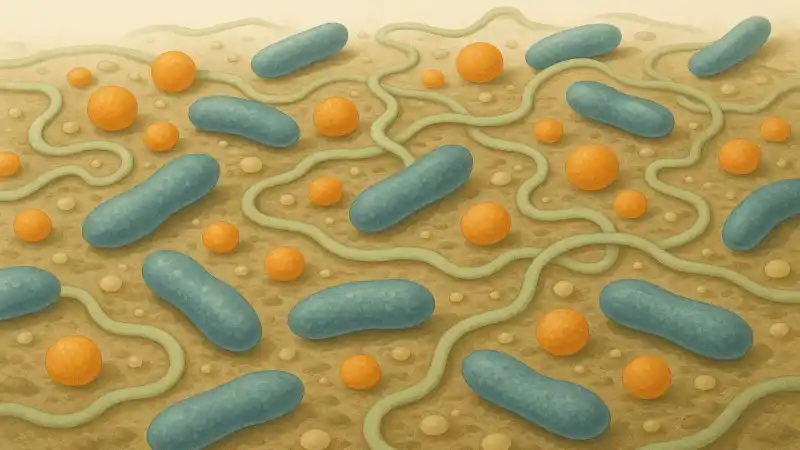
A lot of people notice something small after antibiotics: different bowel habits, more gas, a new food that suddenly feels “off.” This isn’t one single event with one single timeline. It varies by drug, dose, and the person. But the core mechanism is straightforward. Antibiotics don’t only hit the bacteria causing an infection. They also hit parts of the gut community that help break down fiber, train the immune system, and crowd out opportunists. After a typical course—say amoxicillin after a dental infection or azithromycin for bronchitis—the gut ecosystem is reshuffled, sometimes within days.
The overlooked detail is that the change isn’t just “less bacteria.” It’s a change in which bacteria are left, what they can eat, and what chemicals they produce. That chemical output matters because the gut is a chemical factory. A small shift in who’s making what can feel big in the body.
What gets knocked down, and what slips through

Different antibiotics hit different targets. Broad-spectrum drugs tend to suppress a wider range of species, including helpful anaerobes that thrive without oxygen and are common in the colon. Some bacteria have natural resistance. Others survive because they’re tucked into the mucus layer, embedded in biofilms, or simply in a phase where they’re less vulnerable. So the “survivors” aren’t random. The treatment selects for them.
This selection changes the gut’s balance of functions. Fiber-fermenters may drop, while bacteria that tolerate oxygen or grow quickly can rise. That can mean fewer short-chain fatty acids like butyrate for a while, and different bile acid handling. People often overlook bile acids, but they’re not just for digesting fat. Gut microbes chemically modify them, and antibiotics can interrupt that, shifting gut motility and the environment other microbes live in.
The first days after the course ends
When the pills stop, the gut doesn’t “reset” like restarting a device. It repopulates through regrowth of what survived, plus microbes reintroduced from food, water, other people, and the mouth. The early rebound can look like a temporary bloom of certain groups because the usual competitors are missing. With fewer checks and balances, some microbes expand fast and then shrink again as the community fills back in.
A concrete example clinicians watch for is antibiotic-associated diarrhea, including cases tied to Clostridioides difficile after drugs like clindamycin or certain cephalosporins. Not everyone gets it, and risk varies, but it shows the basic principle: a disturbed ecosystem can leave room for an opportunist. Even without that specific pathogen, looser stools can happen because carbohydrate fermentation, water handling in the colon, and bile acids can all shift at once.
Months later, it’s often “recovered” but not identical
Over weeks to months, many people’s gut microbiomes move back toward their earlier pattern. But “back toward” doesn’t always mean “the same.” Some species return quickly because they were never fully lost. Others may stay reduced for a long time or disappear locally if they were rare to begin with. The microbiome has redundancy, so functions can come back even if the exact species mix changes.
One detail researchers keep finding is that diversity can drop after antibiotics and then partially rebound, but the rebound can be uneven. Two people can take the same drug and end up with different long-term shifts because their starting communities were different. Diet, age, other medications, and prior antibiotic exposures all shape what “recovery” looks like, and the timing is unclear and variable across studies.
What changes inside the microbes that remain
It isn’t only about which microbes are present. Antibiotics can change the genes that circulate in the gut. Surviving bacteria may carry antibiotic-resistance genes, and those genes can move between microbes through horizontal gene transfer. This can happen in the gut because bacteria swap genetic material surprisingly readily under the right conditions. The community after antibiotics can be shaped by that genetic reshuffling, not just by who lived or died.
The immune system is part of the story too. Microbes constantly signal to gut immune cells, and when the signals change, immune tone can shift. That can influence which microbes are tolerated, which are attacked, and how inflamed or calm the gut lining is. So the “after” state isn’t only a smaller or larger population. It’s a new set of relationships between microbes, chemistry, and the gut wall, and those relationships can keep evolving long after the last dose.